Aldosterone is a vital hormone in the human body, primarily known for its role in regulating sodium and potassium levels, which are critical for maintaining proper fluid balance, blood pressure, and nerve function. Produced by the adrenal glands, aldosterone acts directly on the kidneys to adjust how much sodium and potassium are retained or excreted in urine, a process essential for the body’s homeostasis. This regulation is fundamental to cardiovascular health and helps prevent imbalances that could otherwise lead to serious health issues, such as hypertension or hypokalemia (low potassium levels).
In this article, we will explore aldosterone’s effects on sodium and potassium balance in the body, explaining how this powerful hormone achieves this balance through various mechanisms. Examples will illustrate how changes in aldosterone levels impact health, and why understanding this hormone is crucial for both medical professionals and patients.
Aldosterone: The Basics
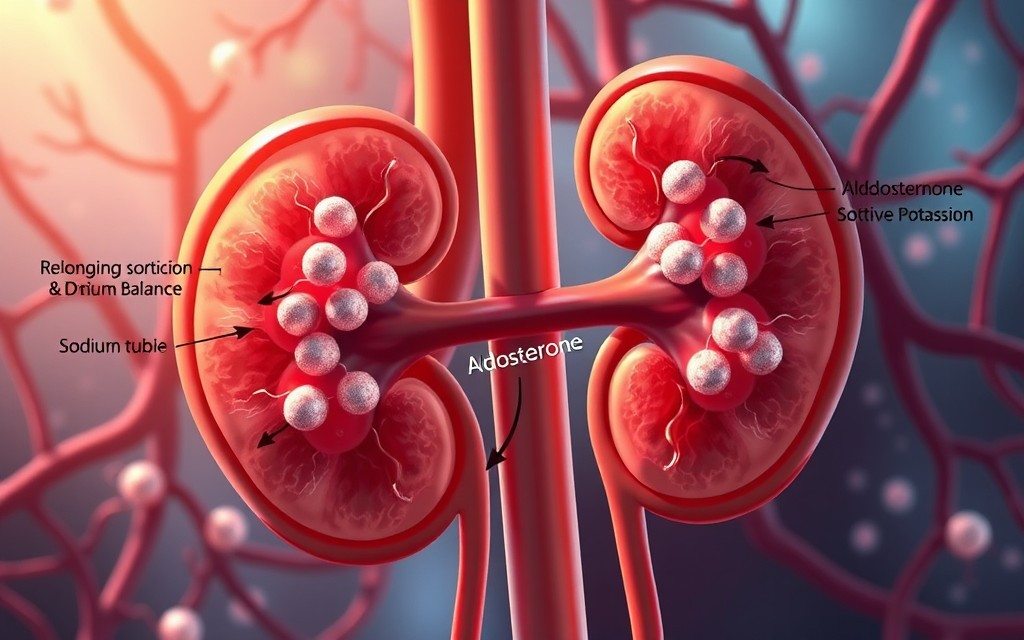
Aldosterone is a mineralocorticoid hormone produced by the adrenal cortex, the outer region of the adrenal glands located above each kidney. It is part of the renin-angiotensin-aldosterone system (RAAS), a complex hormonal network that regulates blood pressure, electrolyte balance, and fluid homeostasis.
When blood volume or blood pressure drops, or when blood potassium levels are high, the kidneys release an enzyme called renin, which initiates a chain reaction. Renin converts a precursor protein into angiotensin I, which is then converted to angiotensin II by the lungs. Angiotensin II stimulates the adrenal glands to release aldosterone. Once released, aldosterone signals the kidneys to adjust sodium and potassium levels in a way that increases blood pressure and restores fluid balance.
Example: Aldosterone Release After Sweating
When we sweat, the body loses both water and sodium. This loss triggers aldosterone production, which helps conserve sodium and retain water to prevent dehydration. This example highlights aldosterone’s role in maintaining fluid balance during activities where we lose fluids, such as exercise or exposure to heat.
Aldosterone and Sodium Balance
Sodium is a critical electrolyte in the body, responsible for maintaining fluid balance, nerve function, and muscle contraction. Aldosterone’s effects on sodium balance are essential for preserving these physiological processes and ensuring that the body functions smoothly.
Sodium Reabsorption in the Kidneys
Aldosterone primarily acts on the kidneys, specifically targeting structures called the distal tubules and collecting ducts. In these parts of the kidney, aldosterone binds to mineralocorticoid receptors, activating a sequence of cellular events that stimulate sodium reabsorption. This process occurs through sodium channels and sodium-potassium pumps, which work together to transport sodium from the urine back into the bloodstream.
As sodium is reabsorbed, water follows due to osmotic pressure, which increases blood volume and consequently raises blood pressure. The process of reabsorbing sodium is one of the body’s primary ways of regulating blood pressure, and aldosterone plays a key role in this function.
Example: Low Blood Pressure and Aldosterone
If blood pressure drops due to dehydration or blood loss, the body releases aldosterone to increase sodium reabsorption in the kidneys. This action draws water back into the bloodstream, increasing blood volume and raising blood pressure to healthier levels. For example, after significant fluid loss from vomiting or diarrhea, aldosterone acts to retain as much sodium and water as possible to restore proper blood volume.
Sodium Retention and Hypertension
In cases where aldosterone levels are abnormally high, sodium retention can become excessive, leading to elevated blood pressure, a condition known as hypertension. Conditions such as hyperaldosteronism (excess aldosterone production) cause the body to retain more sodium and water than necessary, resulting in consistently high blood pressure. This is often associated with symptoms such as headaches, fatigue, and, in severe cases, heart and kidney damage.
Example: Primary Hyperaldosteronism and Sodium Retention
Primary hyperaldosteronism, also called Conn’s syndrome, is a condition in which the adrenal glands produce too much aldosterone, causing excessive sodium retention and high blood pressure. Patients with this condition often present with hypertension resistant to standard treatments, as well as muscle weakness and fatigue. Treating hyperaldosteronism typically involves medication or surgery to reduce aldosterone production and control blood pressure.
Aldosterone and Potassium Balance
While aldosterone increases sodium reabsorption, it has the opposite effect on potassium. Proper potassium balance is vital for muscle and nerve function, heart rhythm, and various cellular processes. Aldosterone promotes the excretion of potassium in urine, thus lowering potassium levels in the blood. This is critical for preventing hyperkalemia, a condition characterized by elevated blood potassium that can lead to dangerous heart arrhythmias.
Potassium Secretion in the Kidneys
In the same kidney regions where aldosterone increases sodium reabsorption, it simultaneously promotes potassium secretion. When aldosterone binds to receptors in the distal tubules and collecting ducts, it enhances the activity of sodium-potassium pumps. These pumps bring sodium into the blood while moving potassium from the blood into the kidney tubules. The potassium is then excreted in the urine, helping to maintain a safe balance of potassium in the body.
Example: High Potassium Levels and Aldosterone Release
Aldosterone is released in response to elevated potassium levels, a common occurrence after a meal high in potassium-rich foods like bananas, oranges, or potatoes. When blood potassium levels rise, aldosterone helps excrete the excess potassium, preventing levels from becoming dangerously high and ensuring proper cellular function.
Risks of Low Aldosterone and Hyperkalemia
In situations where aldosterone levels are low, potassium excretion can be insufficient, resulting in hyperkalemia (high blood potassium). This condition is potentially life-threatening, as high potassium levels can disrupt normal heart function and lead to arrhythmias or even cardiac arrest. Disorders such as Addison’s disease, which involves adrenal insufficiency, can result in low aldosterone levels and an increased risk of hyperkalemia.
Example: Addison’s Disease and Potassium Imbalance
In Addison’s disease, the adrenal glands fail to produce adequate aldosterone, leading to decreased sodium retention and insufficient potassium excretion. Patients with Addison’s disease often experience symptoms like muscle weakness, fatigue, and irregular heartbeats due to an imbalance in sodium and potassium. Treatment usually involves hormone replacement therapy to restore normal aldosterone levels and maintain balanced electrolyte levels.
The Interplay Between Sodium and Potassium Regulation
Aldosterone’s effects on sodium and potassium balance are closely linked through its actions in the kidneys. When aldosterone promotes sodium reabsorption, it simultaneously enhances potassium excretion. This balance ensures that the body maintains optimal electrolyte concentrations, which are crucial for nerve transmission, muscle contraction, and maintaining stable blood pressure.
Example: The Sodium-Potassium Pump
The sodium-potassium pump is a cellular mechanism in the kidneys that aldosterone activates to regulate both sodium and potassium. The pump moves three sodium ions out of the cells into the blood while transporting two potassium ions into the cells, which are later excreted. This mechanism is essential for maintaining electrolyte balance and ensuring normal cellular function.
This simultaneous action on both sodium and potassium demonstrates aldosterone’s efficiency in maintaining equilibrium. By keeping both ions in balance, aldosterone prevents issues related to excess or deficiency, thus supporting cardiovascular and overall cellular health.
Health Implications of Aldosterone Imbalance
Aldosterone levels that are too high or too low can have serious health consequences due to their effects on sodium and potassium regulation.
Hyperaldosteronism: High Aldosterone Levels
Excessive aldosterone production, as seen in conditions like primary hyperaldosteronism or Conn’s syndrome, leads to excessive sodium retention and increased potassium excretion. Over time, this imbalance can result in sustained hypertension and hypokalemia (low blood potassium levels), both of which are associated with significant health risks.
- Hypertension: Chronic sodium retention raises blood pressure, increasing the risk of heart disease, stroke, and kidney damage.
- Hypokalemia: Low potassium levels can cause muscle weakness, cramps, fatigue, and in severe cases, life-threatening heart arrhythmias.
Example: The Risks of Untreated Hyperaldosteronism
If left untreated, hyperaldosteronism can cause significant damage to the cardiovascular system, leading to chronic high blood pressure and the potential for stroke, heart attack, or kidney disease. Patients often require medications that block aldosterone or surgical removal of the adrenal tumor to restore normal aldosterone levels.
Hypoaldosteronism: Low Aldosterone Levels
On the other hand, insufficient aldosterone, as seen in adrenal insufficiency or Addison’s disease, leads to inadequate sodium retention and reduced potassium excretion, resulting in hyponatremia (low sodium levels) and hyperkalemia.
- Hyponatremia: Low sodium levels can lead to dehydration, low blood pressure, fatigue, and confusion.
- Hyperkalemia: Excess potassium in the blood increases the risk of heart complications, as it interferes with normal heart rhythm and muscle function.
Example: Addison’s Disease and Its Symptoms
Patients with Addison’s disease often exhibit symptoms such as low blood pressure, extreme fatigue, weight loss, and darkening of the skin due to insufficient aldosterone. To correct these imbalances, hormone replacement therapy (including aldosterone-like drugs) is typically administered, restoring normal sodium and potassium levels.
Conclusion: The Vital Role of Aldosterone in Sodium and Potassium Balance
Aldosterone plays a critical role in maintaining the delicate balance of sodium and potassium in the body. By regulating these electrolytes, it supports blood pressure control, fluid balance, and proper muscle and nerve function. Aldosterone achieves this balance through its effects on the kidneys, promoting sodium retention and potassium excretion.
The consequences of aldosterone imbalance underscore the hormone’s importance. Excess aldosterone can lead to hypertension and hypokalemia, while low aldosterone may cause dehydration, low blood pressure, and hyperkalemia. Through its actions, aldosterone ensures that the body’s electrolytes remain within safe ranges, making it a cornerstone of health and homeostasis.
As we continue to understand the broader implications of aldosterone, it becomes evident that this hormone is vital not only for regulating blood pressure but also for maintaining the balance necessary for cellular function and long-term cardiovascular health.