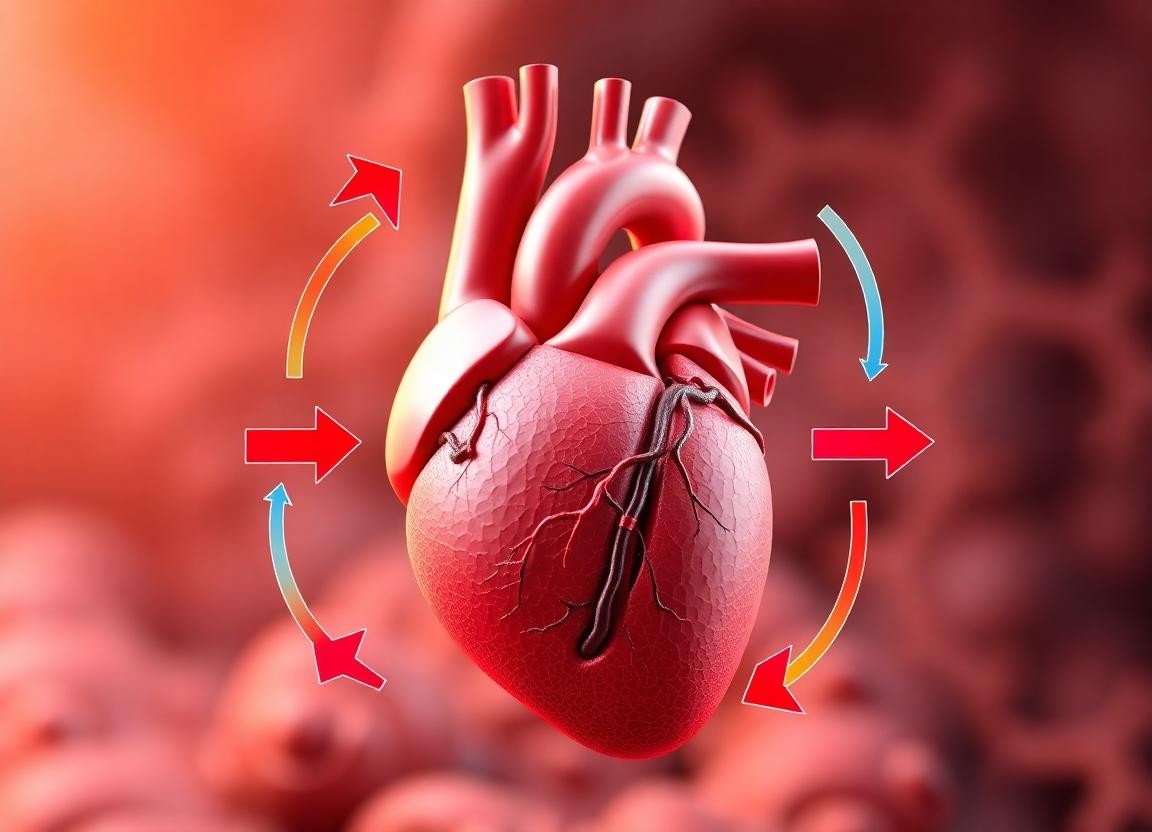
The cardiac cycle is a series of events that occur during one complete heartbeat, encompassing the contraction and relaxation of the heart muscles. This cycle is essential for maintaining effective blood circulation throughout the body, ensuring that oxygen and nutrients are delivered to tissues while waste products are removed. The cardiac cycle can be divided into distinct phases, each characterized by specific mechanical and electrical activities. This article will explore the phases of the cardiac cycle in detail, including the events that occur during each phase, the role of the heart’s electrical conduction system, and examples to illustrate each concept.
1. Overview of the Cardiac Cycle
The cardiac cycle consists of two main phases: systole and diastole. Systole refers to the phase of contraction, during which the heart pumps blood out of the chambers, while diastole refers to the phase of relaxation, during which the heart chambers fill with blood. The entire cycle is regulated by the heart’s electrical conduction system, which coordinates the timing of contractions and relaxations.
2. Phases of the Cardiac Cycle
The cardiac cycle can be further divided into several specific phases, each with distinct events:
A. Atrial Systole
Atrial systole is the first phase of the cardiac cycle, occurring at the end of diastole. During this phase, the atria contract, pushing blood into the ventricles.
- Electrical Activity: The sinoatrial (SA) node, located in the right atrium, generates an electrical impulse that spreads through the atria, causing them to contract.
- Blood Flow: As the atria contract, blood is forced through the atrioventricular (AV) valves (the tricuspid and mitral valves) into the ventricles.
Example: Atrial Systole in Action
Consider a scenario where the heart is at rest. As the SA node fires, the electrical impulse travels through the atria, leading to their contraction. This contraction forces blood from the right atrium into the right ventricle and from the left atrium into the left ventricle. This phase accounts for approximately 20-30% of the total ventricular filling, ensuring that the ventricles are adequately filled with blood before the next phase.
B. Isovolumetric Contraction
Following atrial systole, the ventricles begin to contract in a phase known as isovolumetric contraction. During this phase, the ventricles contract, but the volume of blood within them remains constant because all heart valves are closed.
- Electrical Activity: The electrical impulse from the SA node travels to the atrioventricular (AV) node, then through the bundle of His and Purkinje fibers, leading to ventricular contraction.
- Pressure Changes: As the ventricles contract, the pressure within them rises sharply, but the AV valves remain closed, preventing blood from flowing back into the atria.
Example: Isovolumetric Contraction Dynamics
Imagine the ventricles contracting after the atria have emptied their blood. The pressure in the ventricles increases as the heart muscle contracts, but since the AV valves are closed, no blood is ejected yet. This phase is crucial for building pressure before the next phase, where blood is ejected into the arteries. The isovolumetric contraction phase lasts only a brief moment, typically around 0.05 seconds.
C. Ventricular Ejection
Ventricular ejection is the phase during which blood is expelled from the ventricles into the pulmonary artery and aorta.
- Opening of Semilunar Valves: When the pressure in the ventricles exceeds the pressure in the aorta and pulmonary artery, the semilunar valves (the aortic and pulmonary valves) open.
- Blood Flow: Blood is ejected from the right ventricle into the pulmonary artery and from the left ventricle into the aorta.
Example: Ventricular Ejection in Action
During vigorous physical activity, such as running, the heart rate increases, and the ventricles contract more forcefully. As the left ventricle ejects blood into the aorta, it delivers oxygen-rich blood to the body. The right ventricle sends deoxygenated blood to the lungs for oxygenation. This phase is critical for maintaining adequate blood flow to meet the body’s metabolic demands.
D. Isovolumetric Relaxation
After ventricular ejection, the heart enters the isovolumetric relaxation phase. During this phase, the ventricles relax, and the pressure within them decreases, but the volume of blood remains constant as all valves are closed.
- Pressure Changes: The ventricles begin to relax, causing the pressure to drop. The semilunar valves close to prevent backflow of blood from the aorta and pulmonary artery.
- Electrical Activity: The heart’s electrical activity is at a low point, and the heart prepares for the next cycle.
Example: Isovolumetric Relaxation Dynamics
Following a period of intense exercise, the heart experiences isovolumetric relaxation as it prepares for the next heartbeat. The closure of the semilunar valves prevents blood from flowing back into the ventricles, allowing them to relax without changing volume. This phase is essential for ensuring that the heart is ready to fill with blood again during the next diastole.
E. Ventricular Filling
Ventricular filling occurs during diastole when the heart chambers fill with blood in preparation for the next contraction.
- Opening of AV Valves: As the pressure in the atria exceeds that in the ventricles, the AV valves open, allowing blood to flow from the atria into the ventricles.
- Passive and Active Filling: Ventricular filling occurs in two phases: passive filling (when blood flows into the ventricles due to pressure differences) and active filling (during atrial systole).
Example: Ventricular Filling in Action
After the heart has relaxed, blood from the veins returns to the atria. As the atria fill, the pressure increases, causing the AV valves to open. Blood flows passively into the ventricles, and during atrial systole, the remaining blood is actively pushed into the ventricles. This phase is crucial for ensuring that the ventricles are adequately filled with blood before the next contraction.
3. Summary of the Cardiac Cycle Phases
To summarize, the cardiac cycle consists of the following phases:
- Atrial Systole: Atria contract, pushing blood into the ventricles.
- Isovolumetric Contraction: Ventricles contract with closed valves, increasing pressure.
- Ventricular Ejection: Blood is ejected from the ventricles into the arteries.
- Isovolumetric Relaxation: Ventricles relax with closed valves, decreasing pressure.
- Ventricular Filling: Blood flows from the atria into the ventricles, preparing for the next cycle.
4. Importance of the Cardiac Cycle
Understanding the phases of the cardiac cycle is essential for several reasons:
- Clinical Relevance: Knowledge of the cardiac cycle is crucial for diagnosing and treating cardiovascular diseases. Abnormalities in any phase can indicate underlying health issues, such as heart failure or valve disorders.
- Physiological Insights: The cardiac cycle provides insights into how the heart adapts to varying physiological demands, such as during exercise or rest. For example, during exercise, the heart rate increases, leading to shorter diastolic filling times, which can affect cardiac output.
- Research and Innovation: Advances in medical technology, such as echocardiography and cardiac imaging, rely on understanding the cardiac cycle to assess heart function and guide treatment decisions.
Conclusion
The cardiac cycle is a complex and dynamic process that ensures the efficient functioning of the heart and the effective circulation of blood throughout the body. By understanding the distinct phases of the cardiac cycle—atrial systole, isovolumetric contraction, ventricular ejection, isovolumetric relaxation, and ventricular filling—we gain valuable insights into the heart’s rhythmic function and its critical role in maintaining overall health. As research continues to advance our understanding of cardiovascular physiology, the knowledge of the cardiac cycle will remain fundamental to both clinical practice and the ongoing quest to improve heart health and prevent cardiovascular diseases.